Etiology and pathogenesis of pulpitis
Tradução automática
O artigo original está escrito em RU language (link para lê-lo).
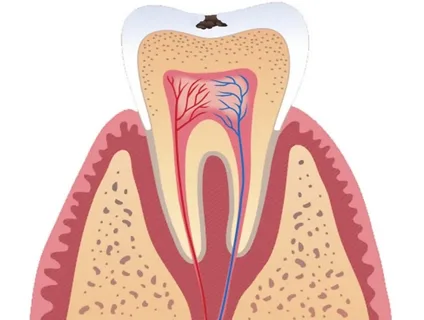
The dental pulp is a collection of connective tissue, loose, with an abundance of fibers, blood vessels and nerves, which fills the space of the tooth cavity.
The reasons contributing to the development of pulp inflammation may be the following:
injury,
bacterial invasion,
chemical exposure,
iatrogenic factor,
denticles,
idiopathic cause.
Learn more about the treatment of pulpitis in primary teeth at the webinar Treatment of the pulp of primary teeth. When? How?
Bacterial invasion
The inflammatory reaction of the dental pulp is the result of exposure to microorganisms, as well as the products of their metabolism.
Bacterial agents that predominantly cause pulpitis:
Streptococci occupy the first place, the vast majority of them are sown;
other pyogenic cocci,
fusospirochetes,
gram-positive rods,
mushrooms.
Most often, the pathogenic microflora penetrates the tissues of the pulp chamber orthogradely, from the side of the carious cavity of the tooth. But we should not exclude another route of penetration – retrograde, from the periodontal tissues.

Rice. 1. Dental pulp.
Factors contributing to retrograde penetration of infection:
exacerbation of periodontal disease,
due to flap surgery,
with osteomyelitis,
as a complication of capillary toxicosis.
Trauma as an etiological factor of pulpitis
Inflammatory damage to the dental pulp tissue can develop as a result of acute or chronic trauma.
Acute trauma that can cause pulpitis:
fractures or cracks in the crown or root of a tooth,
tooth subluxation,
complete dislocation
vertical tooth fracture.
As a result of an acute injury, the tooth cavity is opened, and then the pulp tissue is infected with pathogenic microflora from the oral cavity.
Etiological factors that can lead to chronic inflammation of the pulp:
pathological abrasion,
bad habits,
occupational hazards,
bruxism.
Chemical exposure
Substances that have a toxic effect on dental pulp:
restoration materials,
materials for gaskets,
pickling agents
alcohols, phenols, ether.
Iatrogenic factor
Performing a number of dental procedures can cause the development of an inflammatory response of the dental pulp. At different stages of treatment, the dentist may make mistakes that will serve as an iatrogenic etiological factor in the development of pulpitis.
Errors at the preparation stage
excessive pressure on the tissue being prepared,
lack of adequate air-water cooling,
active preparation without interruption,
non-compliance with the recommended preparation regimen at different stages.

Rice. 2. Neurovascular bundle.
Errors at the stage of working with restoration material
overdrying of dentin or insufficient drying;
too long exposure of the etching agent during total etching,
poor-quality marginal fit of the restoration.
At the stage of treatment of periodontal diseases, surgical intervention on periodontal tissues, damage to the vessels leading to the pulp may occur, which will provoke the development of retrograde pulpitis.
The creation of excessive pressure on the teeth during orthodontic treatment causes external root resorption, and as a result, damage to the pulp.
Errors in the process of orthopedic treatment that cause the development of pulp inflammation
preparation for a crown without taking into account the topography of the pulp chamber and safety zones,
excessive convergence of tooth walls during preparation for various orthopedic structures,
planning the design without taking into account the age characteristics of the patient,
treatment without applying temporary crowns.
Idiopathic pulpitis
Inflammatory phenomena in the pulp can develop for unknown, idiopathic reasons. Thus, some clinicians observed pulpal pain in a patient with herpes zoster. Also, the cause of internal granuloma has not yet been clarified.
Pathogenesis of pulpitis
In the pulp tissues, as a result of exposure to a damaging factor, a number of vascular-tissue responses are triggered:
biochemical,
structural,
histochemical.
The severity of these reactions is determined by the body’s defenses and the state of its nervous system.
The inflammatory response, regardless of the etiological factor, includes the following stages: alteration, exudation, proliferation.
Rice. 3. Prerequisites for the development of pulpitis.
First stage of alteration
Increased phagocytic activity of monocytes and polymorphonuclear neutrophils.
Release of inflammatory mediators.
Oxygen in active forms accumulates in tissues.
The pH value shifts towards an acidic environment, which causes destruction of cellular structures.
Hydrolytic enzymes, when released, destroy protein substrates.
Potassium ions, released as a result of damage to pulp cells, change the electrolyte balance, disrupt the tone of the nervous system, and lead to an increase in hyperemia.
During acute inflammation, the activity of enzymes in the dental pulp increases.
Enzyme activity during chronic inflammation drops sharply, which indicates a slowdown in metabolic processes in the pulp.
Second stage of exudation
This is a vascular response of pulp tissue, which is predominantly expressed in its coronal region. An excess of inflammatory mediators causes a reflex spasm of microvessels, but this phenomenon is short-term in nature, quickly followed by dilation of arterioles and capillaries. The flow of blood and lymph slows down, vascular permeability increases, and blood cells and part of the plasma are released into the pulp tissue. This is how exudate is formed.
Third stage of proliferation
This stage of the inflammatory reaction is aimed at saving damaged pulp tissues; the greatest intensity of the processes is observed in the root area. In the pulp, the cellular composition changes, hyalinosis of collagen fibers, active division of cells in the central layer, and fibrosis of the root pulp occur.
The pulp contains thin connective tissue fibers, an abundance of dilated thin-walled capillaries, a root pulp with a poor cell composition, and degeneration of collagen fibers.
Denticles
The collective term "pulp degeneration" includes the following formations, calcified structures that can occur in pulp tissue:
denticles,
pulp stones,
calcifications.
Denticles are benign formations that are located in the pulp chamber; they are characterized by a constant increase in size.

Rice. 4. Intact pulp.
Highly organized, they are also called true, denticles are surrounded along the edge by odontoblasts and have dentinal tubules. Their structure is similar to that of healthy dentin.
False denticles are more common in terms of frequency of occurrence. They are a conglomerate of calcified material that does not contain dentinal tubules.
The denticle can be located freely (free-lying), it is completely surrounded by pulp tissue, can be attached to the wall - parietal, or can be immersed in dentin - interstitial.
Denticles are so large that they completely obliterate the root canals and tooth cavity.
Petrificates are zones of calcification, which are most often found in the root of the tooth; they are located along the periphery of blood vessels and nerves.
Causes of pulp calcifications
Hereditary.
Physical and chemical effects: excessive load in the form of traumatic occlusion or functional inaction in case of retention, wedge-shaped defects, preparation for an orthopedic structure, metal filling.
Trauma – bruise, dislocation, fracture, excessive orthodontic load.
Metabolic disorders.
Age.
Petrificates and denticles are found in pulp tissues in patients of any age, regardless of the jaw affiliation of the tooth, in permanent and temporary teeth, even in intact teeth with healthy periodontium.
Despite the fact that the prevalence of dental damage by denticles is about 40-50%, there are no clinical manifestations in patients.
In rare cases, petrificates and denticles cause paroxysmal intense pain; in such a situation, the patient will be diagnosed with concremental pulpitis, which is confirmed by x-ray examination.
On an x-ray, denticles against the background of the pulp chamber or root canal appear as areas of intense shadow, having rounded, elongated or irregular outlines.
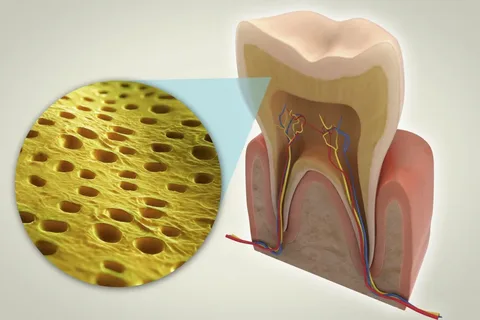
Rice. 5. Longitudinal section of the tooth.
Petrifications with lower density and degree of calcification are not visualized in the image.
A dentist, when performing endodontic treatment of a tooth with denticles and petrificates, must take into account the following factors:
Devitalization of such teeth is not very effective due to mechanical obstacles in the path of the devitalizing drug.
The use of local anesthetics is often ineffective.
Atypical localization of the tooth cavity and canal orifices.
More detailed up-to-date information on this topic at the webinar Pulp preservation: a science-based approach .

