Use of Botulinum Toxin Before Surgical Lip Repositioning: A Randomized Clinical Trial
Abstract
This study aimed to determine whether administering botulinum toxin type A (BT) prior to surgery would stabilize surgical lip repositioning. And more details about periodontal surgery treatment protocols are accessible for you to learn on our website in Parodontology section.
A randomized controlled parallel-group clinical trial was performed. A total of 18 participants with excessive gingival display (EGD) were divided into two groups. For the test group (TG), BT was injected into the smile muscle locations 15 days before the surgical procedure. For the control group (CG), only lip repositioning surgery was performed. Gingival display (GD) and upper lip displacement (LD) were measured 3 and 6 months postoperatively. Data were submitted to ANOVA, Tukey, and t tests. For GD and LD, the changes were statistically significant between the measurements taken at the baseline, 3-month, and 6-month marks. The GD presented a reduction of 5.2 ± 1.1 mm in TG and 3.2 ± 1.4 mm in CG after 6 months. The LD measurements reduced 45% for TG and 26% for CG in 6 months. The injection of BT 15 days before lip repositioning surgery provided more stable results and effectively reduced the GD at 6 months.
Introduction
The growing interest of patients in esthetic procedures, as well as the development of less invasive protocols in dentistry, has promoted the development of treatment plans that include stability, harmony, and function in orofacial rehabilitation. Poor esthetics interfere with an individual’s personal, social, and professional relationships and is an individual consideration that varies according to the patient’s age, time, region, and culture concerning what is considered beautiful.(1)
Excessive gingival display (EGD) can be classified as gingival exposure above 1.5 mm when smiling, but the consensus among laymen and dental professionals is that over 3 mm is unattractive.2–5 EGD is a common complaint that affects 10% of the population aged 20 to 30 years, with a higher prevalence among women.(6) The incidence of this condition gradually decreases with age as a consequence of decreased upper and lower lip muscle tone, which in turn leads to a decrease in maxillary tooth exposure and an increase in mandibular tooth exposure.(7) The etiology of EGD can be dental, skeletal, muscular,8 or, recently, classified as a dentoalveolar or nondentoalveolar discrepancy.(9)
Thus, for optimal treatment planning, a correct diagnosis is essential. Upper lip hyperactivity is mainly related to the action of the lip lifter muscles and is diagnosed by assessing lip dislocation when smiling. Where the normal pattern of lip dislocation is between 6 and 8 mm, the hyperactive lip is 1.5 to 2 times longer than the normal lip—that is, 9 mm or more.(10–12)
Spontaneous smiles are the action of the upper lip lifter, while voluntary smiles are the action of the greater zygomatic and buccinator fibers in addition to the upper lip lifter.(13) Upper lip hyperfunction has been treated surgically via muscle myectomy or other less-invasive treatments, such as surgical lip repositioning.(14,15) Nonsurgical therapies have also been used, such as the injection of botulinum toxin type A (BT).(16–18)
Surgical lip repositioning, described by Rubinstein and Kostianovsky(14) and modified by Ribeiro-Júnior et al,(19) aims to limit retraction of the lip elevator muscles. This technique removes a mucosa band from the upper vestibule, and the labial mucosal is sutured from the mucogingival junction. This method is widely used despite its recurrence rate,(9) as it is less invasive than other surgical options.
BT has been used since the late 1970s to treat various conditions associated with excessive muscle contraction or pain.(20) In 2005, Polo undertook a pilot project for the use of BT in the upper lip musculature and concluded that the therapy is effective, temporary, and minimally invasive.(16) The duration of toxin action for EGD varies from 2 to 3 months.(21)
To reduce the relapse associated with repositioning surgery and to provide a lasting treatment without the need for reapplication, as in the case of the toxin, a combined treatment using the toxin preoperatively was considered. Thus, the purpose of this clinical study was to evaluate the effectiveness of an integrated care protocol associating the previous application of BT with the surgical lip repositioning technique used to treat EGD.
Materials and Methods
Study Design
This study adopted the Consolidated Standards of Reporting Trials (CONSORT) guidelines, and the trial was registered as RBR-2f5msy in the Brazilian Registry of Clinical Trials. All participants were aware of the study design and signed an informed consent approved by the Ethical Committee of the University Veiga de Almeida on October 10, 2018 (no. 2.955.631), and was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013.
This study focused on the prognosis, and the intervention design was parallel, two-armed, nonmasked, randomized, and controlled. The randomization was carried out through sealed envelopes divided and distributed among the total number of research participants to determine group allocation. Each participant removed their group allocation from the envelope and observed which treatment they would receive. The sample size was calculated by means of the standard deviation in a previous study,(9) taking gingival exposure into account. The result was a sample size of 14, with a confidence level of 95% and a sampling error of 5%. The sample size was increased to 18 individuals to account for dropouts. The sample was divided into two groups as follows: test group (TG) = at 15 days before the lip repositioning surgery, BT was injected in points associated with the levator labii superior alaeque nasi/levator labii superioris (LLSAN/LLS), zygomaticus minor (Zmi), and levator labii superioris (LLS) muscles; and control group (CG) = the lip repositioning surgery was performed without any prior application of BT. The procedures were performed by examiner 1 (K.B.A.), who was responsible for monitoring initial and final measurements; examiner 2 (A.D.), who was responsible for applying BT; and examiner 3 (S.K.), who was responsible for all upper lip repositioning surgeries.
Inclusion/Exclusion Criteria
Inclusion criteria were as follows: Patients (1) had gingival exposure greater than 3 mm when smiling, (2) had a hyperactive upper lip with or without other causes of EGD (lip displacement ≥ 9 mm), (3) were adults between 18 and 50 years old, and (4) were systemically and periodontally healthy.
Exclusion criteria were as follows: (1) smoking; (2) pregnancy or lactation; (3) systemic diseases; (4) neuromuscular, neurological, or psychological disorders or consumption of controlled medication; (5) alcohol or drug abuse; (6) periodontal disease or short lip; and (7) those who declined the informed consent or who did not consent to the risks described.
Diagnosis
Clinical measurements were made of the upper lip displacement, lip height, gingival exposure, clinical crown size, and resting and sealed lip exposure to determine the possible etiology of the EGD. Lip displacement was measured from where the lower portion of the lip touched the tooth in the resting position to the final distance of the maximum smile, which was marked with a pen on the tooth and then measured with a periodontal probe (Figs 1a and 1b). Measurement of gingival exposure was standardized from the cervical margin of the maxillary right central incisor to the lip with a probe (Hu-Friedy) at maximum smile (Fig 1c). Front-facing photos of openmouthed smiles, closed-mouth smiles, and the closed-mouth resting position were taken at the initial consultation (baseline), during treatment, 15 days after intervention, and after 3 and 6 months. These photographs were used to check differences after the surgery; no measurements were taken.
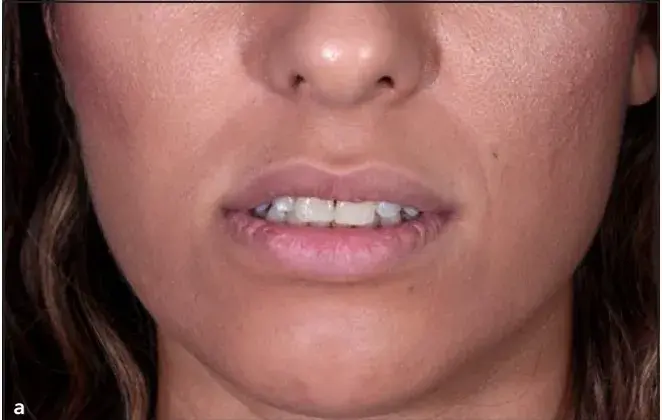

 Fig 1 (a) The spot where lower portion of the lip touches the tooth at the resting position is noted. (b) Final position of the lip at maximum smile. (c) Gingival exposure was measured from the central cervical margin of the maxillary right central incisor to the lip at maximum smile.
Fig 1 (a) The spot where lower portion of the lip touches the tooth at the resting position is noted. (b) Final position of the lip at maximum smile. (c) Gingival exposure was measured from the central cervical margin of the maxillary right central incisor to the lip at maximum smile.
Botulinum Toxin Injection
Onabotulinum toxin-A (Botox, Allergan) was diluted according to the manufacturer’s recommendations by adding 1.0 mL sterile saline solution to 50 units of BT. Under sterile conditions, 6 international units were injected only once per side to the target locations, and 2 units per muscle were injected in the LLSAN/LLS, Zmi, and LLS muscles. To ensure accurate muscle location, the injection sites were determined using a skin marker (Fig 2). The volunteers were advised to avoid lying down, exercising, or massaging the injection area until 4 hours postoperation.
 Fig 2 Two units of toxin injected into each marked point: LLSAN (inner/nose dot), LLS (middle dot), and Zmi (outer/cheek dot).
Fig 2 Two units of toxin injected into each marked point: LLSAN (inner/nose dot), LLS (middle dot), and Zmi (outer/cheek dot).
Lip Repositioning Surgery
Participants were anaesthetized by the infiltration technique and bilateral infraorbital nerve block (2% lidocaine with 1:100,000 epinephrine; Alphacaine, DFL). The amount of mucosa to be removed was marked with a sterile mucosal surgery pen. A horizontal incision was made with a 15C blade from the mesial line angle of the maxillary first molar to the incisor, 1 mm coronal to the mucogingival line. Two vertical incisions at the extremities of the first incision were made corresponding to double the gingival exposure presented at the initial consultation (baseline), or 10 mm apically at most. Finally, an incision parallel to the first connected the vertical incisions. The incision was sufficiently deep to remove the epithelium, but the underlying connective tissue was kept intact. The procedure was repeated on the contralateral side, leaving the frenum intact, which helped stabilize the suture and reposition the upper lip.(19) Simple sutures were used to stabilize the marginal mucosa with the gingival tissue inserted with a 5-0 blue polyamide monofilament suture (Fig 3).


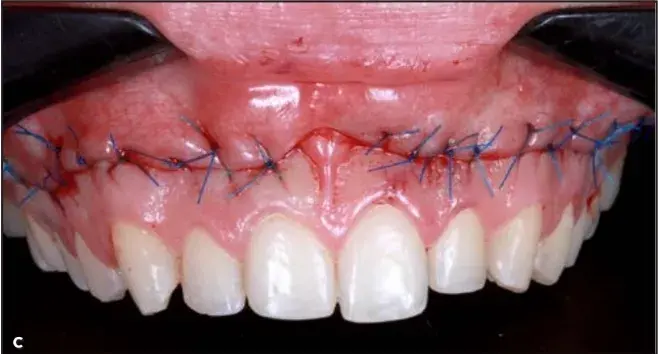 Fig 3 (a) The amount of mucosa to remove was marked with a sterile mucosal surgery pen. (b) The incision was performed, keeping the underlying connective tissue intact. (c) Simple sutures were used to close the surgical site.
Fig 3 (a) The amount of mucosa to remove was marked with a sterile mucosal surgery pen. (b) The incision was performed, keeping the underlying connective tissue intact. (c) Simple sutures were used to close the surgical site.
Postoperative Protocol and Pain Questionnaire
Postoperative guidelines and care included local ice application and the use of analgesics only in case of pain. Medication use, including the doses and times taken postoperatively, was recorded on the pain questionnaire. Postoperative pain was measured with a visual analog scale that ranged from 0 to 10, with 0 indicating no pain and 10 indicating severe pain.
Clinical Outcomes
Outcome measurements included the reduction of lip displacement and the reduction of gingival display (GD) with the participant in maximum smile. All participants answered two questionnaires before and 6 months after the surgery on the impact on quality of life (Oral Health Impact Profile [OHIP-14]) and on esthetic self-perception (Psychosocial Impact of Dental Aesthetics Questionnaire [PIDAQ]). The same clinician (K.B.A.) provided the questionnaires in all cases.
The OHIP-14 assessed seven domains of a patient’s oral health–related quality of life (OHRQoL): functional limitation, physical discomfort, psychological discomfort, physical disability, psychological disability, social disability, and handicaps. Each question was scored on a 5-point Likert scale (1 to 5), with lower scores indicating better OHRQoL and higher scores indicating a worse OHRQoL. The PIDAQ questionnaire measured OHRQoL, comprising 23 questions on four parameters: esthetic concern, phsychologic impact, social impact, and dental self-confidence. Each question was scored on a 5-point scale (0 to 4), with lower scores indicating better OHRQoL and higher scores indicating a worse OHRQoL.
Statistical Analysis
Shapiro-Wilk normality test was applied (α = .05). Results were submitted to analysis of variance (ANOVA) and Tukey test correction and the parametric t test.
Results
A total of 18 participants, all women aged between 20 and 46 years with 5 to 8 mm of GD caused by lip hyperactivity alone or associated with other etiologies, such as altered passive eruption or vertical maxillary excess, were selected for treatment.
In total, 3 participants (16.6%) had a GD of 5 mm, and 15 participants (83.3%) had > 6 mm GD. One participant had an asymmetrical smile. In all cases, upper lip hyperactivity was diagnosed as either a cause alone or associated with another etiology. Some participants had vertical maxillary excess and altered passive eruption as combined causes. Of the 18 participants, 3 (17%) presented isolated upper lip hyperactivity and 15 (83%) had combined causes. The most common cause after upper lip hyperactivity was vertical maxillary excess, at 61%.
Regarding GD at baseline, no statistically significant difference was detected between the groups. According to two-way ANOVA and Tukey test (P < .005), a statistically significant reduction in gingival displacement was detected after 6 months for both groups (Table 1). However, in the TG, the application of BT resulted in a larger reduction of GD values compared with the CG (P < .001) after 6 months.
The mean values of GD reduction were also calculated, and the data initially and after 6 months were submitted to Student t test (Table 2). The application of BT prior to the lip repositioning surgery resulted in a greater reduction of GD compared to the lip repositioning surgery alone (P < .005).
Lip displacement (LD) was measured during maximum smile, and no statistically significant difference was detected between the groups at baseline. After 6 months, the application of BT resulted in a significant reduction of lip displacement compared with CG (Table 3). The reduction in lip displacement for both groups was tested according to the Student t-test (P < .005). The LD was significantly reduced in the TG compared to the CG after 6 months, as the TG had a mean reduction of 4.7 ± 1.5 mm (45% ± 8%), while the mean LD reduction for CG was 2.5 ± 1.5 mm (26% ± 11%) (Table 4).
Table 1 Maximum of Gingival Display According to Treatment Type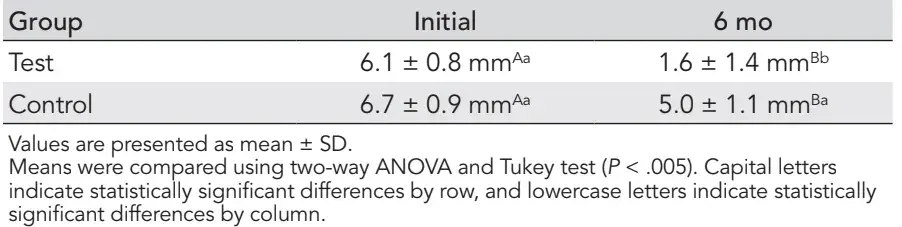
Table 2 Changes in Gingival Display After 6 Months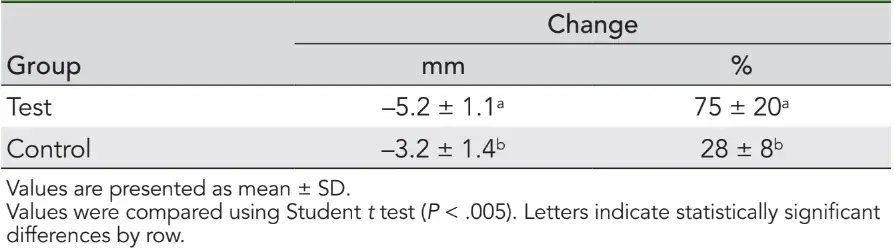
Table 3 Lip Displacement According to Treatment Type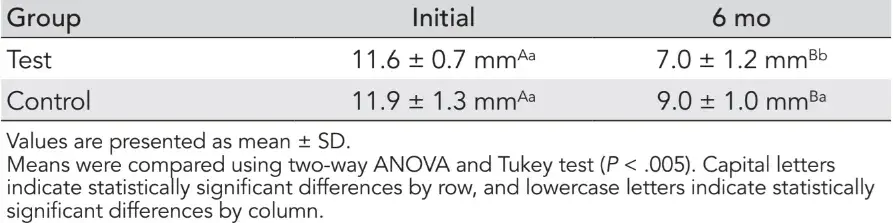
Table 4 Changes in Lip Displacement Reduction After 6 Months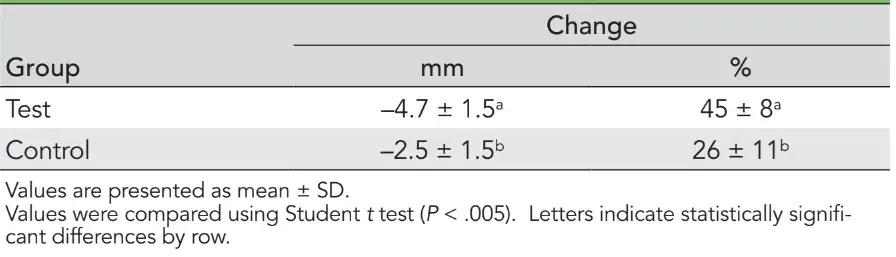
Considering a gingival exposure of > 3 mm as EGD, in the TG, the final TG sample showed an 11% recurrence of EGD after 6 months (one patient with 4 mm of EDG). For the CG, recurrence was 77% at 3 months and 89% at 6 months. Considering lip displacement ≥ 9 mm in the TG, lip hyperactivity was 10% at 3 months and 11% at 6 months. In the CG, lip hyperactivity was 11% at 3 months and 88.9% at 6 months. The mean GD after 6 months showed a difference of more than 3 mm between the TG and CG. The average difference in lip displacement between the TG and CG was 2 mm.
Participants were asked about postoperative pain using a pain questionnaire graded from 0 to 10, where 0 indicates no pain and 10 indicates severe pain. Patients responded to questions about specific pain on the first day, beyond-general pain in the first 15 days, and their level of analgesic use. The average pain score on the first day was 4 ± 3.7 for TG and 3.8 ± 3.2 for CG. Of the patients, 66% used analgesics in TG and 55% used analgesics in CG. The general pain after the surgery was 1.7 ± 1.7 in TG and 1.7 ± 1.6 in CG. No statistically significant differences were detected (Table 5).
Table 5 Mean Pain Score at Follow-ups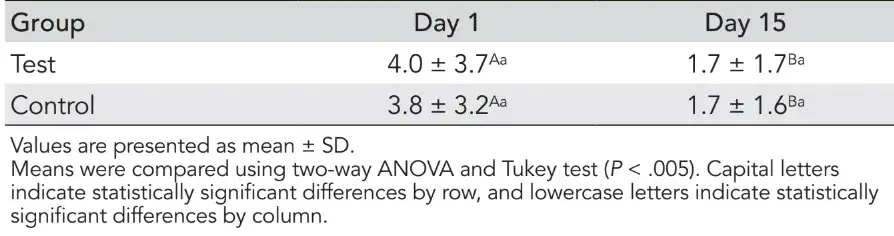
Surgical lip repositioning surgery had a positive impact on the quality of life, especially in the dimension of psychological discomfort, psychological disability, and social disability. Improvements in esthetic self-perception and psychological impact were also seen.
A quantitative evaluation of the sample in the OHIP questionnaire showed an improvement of the initial psychological disability in 100% of the sample (n = 18), with significant improvements in psychological discomfort (77.8%) and social disability (83.3%). The statistical evaluation (chi square test) for each question shows that there was a statistically significant improvement (P = .046) in psychologic discomfort. Normality tests were performed (Kolmogorov-Smirnov and Shapiro-Wilk) to evaluate the OHIP-14 score; for paired and nonparametric samples, Wilcoxon test was applied to assess the general and specific scores. P < .005 was considered statistically significant, and a significant result was obtained in four domains of the OHIP-14 (psychologic discomfort, psychologic disability, social disability, and disability) and in the general score. The average total score for both groups was 10.72 ± 7.50 before surgery and 1.00 ± 1.88 after surgery. The parameters psychologic discomfort, psychologic disability, and social disability had the most noticeable differences.
Shapiro-Wilk normality test was performed to assess the PIDAQ score, and all domains obtained a value above 5%. Paired t-test was used to assess all items in the questionnaire. The alpha value established was 5%, and significant differences were seen in all domains of PIDAQ and the general score. For both groups, the average scores before and after surgery were 35.00 ± 11.57 and 21.39 ± 4.63, respectively, demonstrating significant improvement for all domains. A positive impact on psychologic and dental self-confidence was identified in 61% of patients. Photographs were taken for the TG and CG at baseline, 3 months, and 6 months to show the effects of surgery over time (Figs 4 and 5).
 Fig 4 Control group at (a) baseline and at (b) 3 months and (c) 6 months after the procedure.
Fig 4 Control group at (a) baseline and at (b) 3 months and (c) 6 months after the procedure.
 Fig 5 Test group at (a) baseline and at (b) 3 months and (c) 6 months after the procedure.
Fig 5 Test group at (a) baseline and at (b) 3 months and (c) 6 months after the procedure.
Discussion
Intramuscular injection of BT acts by blocking acetylcholine release from nerve endings in motor neurons, causing the temporary chemical denervation of skeletal muscles and a reduction in muscle contraction.(20)
According to Chagas et al,(21) the effect of the BT remains for 2 to 3 months, and therefore participants in the present study were evaluated 3 and 6 months after treatment to detect any remaining effect. The GD and LD recurrence detected in the TG occurred after 3 months and was stable even after 6 months, when no more effect of BT was expected.
The present study shows the high prevalence of lip hyperactivity combined with other etiologies for EGD and could contribute to correct diagnoses and successful treatment. In a study with 56 patients, Andijani and Tatakis(22) reported that 20.8% had altered passive eruption alone, 45.3% had lip hyperactivity only, and 34% had combined altered eruption and hyperactivity, for a total of 80% with lip hyperactivity. Those authors showed the importance of making the correct etiologic diagnosis and suggested that many patients with EGD could benefit from treatment aimed at reducing lip displacement.
In a systematic review, Duruel et al(23) demonstrated that the application of BT at specific points, including LLSAN, LLS, and Zmi, at a concentration of 5 units per side (10 units per patient), reduced EGD, although re-application might be needed. However, reapplication was not included in the present study design, and the use of toxin application points was defined according to the literature. These were considered “ideal” points associated with the movement of the smile, whether spontaneous or forced. Although an ideal smile could not be achieved for all participants, a measurable improvement was observed from the outset for both groups and was documented with the satisfaction questionnaires. A change in the thickness of the lip vermilion border was also perceived and reported by some participants. Tawfik et al(24) reported that the vermilion border had a mean increase of 1.55 ± 0.81 mm and 1.23 ± 0.47 mm after surgical lip positioning.
Complications such as numbness, paresthesia, edema, and ecchymosis have been reported, especially when surgery becomes more invasive.(10,15,24,25) Upper lip repositioning surgery was initially described by Rubinstein and Kostianovsky,(14) and in 2013 was modified by Ribeiro-Júnior et al(19) in a technique that maintained the frenum, generating a lower surgical morbidity and facilitating the repositioning of the symmetrical lip.(19)
A difference of < 1 mm in GD between the conventional technique and the more invasive muscle dissection technique has been reported.(24,25) Although lip repositioning was successful in reducing EGD, its complete elimination was not consistently achieved when the invasive myectomy technique was used.(25) Thus, the less-invasive surgery was chosen for the present study, both to reduce risk and in anticipation of a more stable EGD correction, and a final GD difference of more than 3 mm between groups was recorded. Although both treatments are frequently used separately to treat EGD, the present authors are unaware of a clinical report using this integrated care protocol. The idea was that preoperatively applying BT would ensure muscle relaxation during tissue healing, improving surgical outcomes and decreasing post-operative pain. The present results showed that subjects in the TG had lip hyperactivity at a rate of 10% and 11% at 3 and 6 months, respectively, while the CG had rates of 11% and 88.9%, respectively. The mean CG value after 6 months represented a difference more than 3 mm between the TG and CG. The mean difference in lip displacement between the groups was 2 mm. According to the literature,(9) the estimated mean improvement possible with lip repositioning is 3.4 mm, and using BT 15 days before the surgery can reduce the GD by almost twice what has been reported previously. In the present study, the TG had a mean improvement of 4.5 mm, while the CG had a mean improvement of only 1.7 mm. The effect of the muscle relaxation provided by the 15-day preoperative application of toxin led to better tissue healing, resulting in less muscle traction during the post-operative period. This was mainly because hyperactivity was one of the main causes of EGD in the studied sample. Healing was uneventful, with all participants presenting an imperceptible scar line at the mucogingival junction. The surgery can be considered minimally painful, as the participants did not use preventive analgesics, which were only to be used if necessary. Analgesic use averaged 66% in the TG and 55% in the CG, but with fewer than 2 tablets taken per subject during the 15-day postoperative period. The pain questionnaire showed that the surgery was not considered painful, with the average pain at 1.77 ± 1.62 on a scale from 0 to 10, and the average number of analgesic pills taken was 1.66 ± 1.81. The use of BT did not decrease pain.
Further studies are needed to optimize the BT dosage. Lip repositioning with BT needs to be evaluated over a longer period to demonstrate longer-term stability. Additional studies with a larger sample size are indicated.
Conclusions
The use of BT 15 days before lip repositioning surgery provided more stable results and effectively reduced gingival exposure at 6 months. Improved EGD was achieved in both groups, with the treatment considered straightforward and minimally painful.
If you enjoyed reading this article and would like to explore the surgical protocols of periodontal diseases treatment further, we encourage you to enroll our course "Advanced periodontology: surgical protocols" by Daniel Melker.
Acknowledgments
All authors have made substantial contributions to conception and design of the study. A.K.B., D.A., K.S. were involved in surgery, application of toxin botulinic, data collection and data analysis. A.K.B., S.L.F., C.L.M. were involved in data interpretation, drafting the manuscript and revising it critically, and have given final approval of the version to be published. The authors do not have any financial interests, either directly or indirectly, in the products or information associated with this manuscript.
List of authors:
Karinne Bueno Antunes, Alexandra Dias, Sérgio Kahn, Luiz Felipe Jochims Schneider, Larissa Maria Cavalcante
References
Flores-Mir C, Silva E, Barriga MI, Lagravere MO, Major PW. Lay person’s perception of smile aesthetics in dental and facial views. J Orthod 2004;31:204–209.
Robbins JW. Differential diagnosis and treatment of excess gingival display. Pract Periodontics Aesthet Dent 1999;11:265–272.
Kokich VO, Kokich VG, Kiyak HA. Perceptions of dental professionals and laypersons to altered dental esthetics: Asymmetric and symmetric situations. Am J Orthod Dentofacial Orthop 2006;130:141–151.
Cracel-Nogueira F, Pinho T. Assessment of the perception of smile esthetics by laypersons, dental students and dental practitioners. Int Orthod 2013;11:432–444.
Mokhtar HA, Abuljadayel LW, Al-Ali RM, Yousef M. The perception of smile attractiveness among Saudi population. Clin Cosmet Investig Dent 2015;7:17–23.
Tjan AH, Miller GD, The JG. Some esthetic factors in a smile. J Prosthet Dent 1984;51:24–28.
Silberberg N, Goldstein M, Smidt A. Excessive gingival display—Etiology, diagnosis, and treatment modalities. Quintessence Int 2009;40:809–818.
Garber DA, Salama MA. The aesthetic smile: Diagnosis and treatment. Periodontol 2000 1996;11:18–28.
Tawfik OK, El-Nahass HE, Shipman P, Looney SW, Cutler CW, Brunner M. Lip repositioning for the treatment of excess gingival display: A systematic review. J Esthet Restor Dent 2018;30:101–112.
Simon Z, Rosenblatt A, Dorfman W. Eliminating a gummy smile with surgical lip repositioning. J Cosmetic Dent 2007;23:102–109.
Burstone CJ. Lip posture and its significance in treatment planning. Am J Orthod 1967;53:262–284.
Peck S, Peck L, Kataja M. Some vertical lineaments of lip position. Am J Orthod Dentofacial Orthop 1992;101:519–524.
Seixas MR, Costa-Pinto RA, Araujo TM. Checklist dos aspectos estéticos a serem considerados no diagnóstico e tratamento do sorriso gengival. Dental Press J Orthod 2011;16:131–157.
Rubinstein A, Kostianovsky A. Cosmetic surgery for the malformation of the laugh: Original technique [in Spanish]. Prensa Med Argent 1973;60:952–954.
Miskinyar SA. A new method for correcting a gummy smile. Last Reconstr Surg 1983;72:397–400.
Polo M. Botulinium toxin type A in the treatment of excessive gingival display. Am J Orthod Dentofacial Orthop 2005;127:214–218.
Polo M. Botulinum toxin type A (Botox) for the neuromuscular correction of excessive gingival display on smiling (gummy smile). Am J Orthod Dentofacial Orthop 2008;133:195–203.
Sucupira E, Abramovitz A. A simplified method for smile enhancement: Botulinum toxin injection for gummy smile. Plast Reconstr Surg 2012;130:726–728.
Ribeiro-Júnior NV, Campos TV, Rodrigues JG, Martins TM, Silva CO. Treatment of excessive gingival display using a modified lip repositioning technique. Int J Periodontics Restorative Dent 2013;33:309–314.
Hwang WS, Hur MS, Hu KS, et al. Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod 2009;79:70–77.
Chagas TF, Almeida NV, Lisboa CO, Ferreira DMTP, Mattos CT, Mucha JN. Duration of effectiveness of Botulinum toxin type A in excessive gingival display: A systematic review and meta-analysis. Braz Oral Res 2018;32:e30.
Andijani RI, Tatakis DN. Hypermobile upper lip is highly prevalent among patients seeking treatment for gummy smile. J Periodontol 2019;90:256–262.
Duruel O, Ataman-Duruel ET, Tözüm TF, Berker E. Ideal dose and injection site for gummy smile treatment with botulinum toxin-A: A systematic review and introduction of a case study. Int J Periodontics Restorative Dent 2019;39:e167–e173.
Tawfik OK, Naiem SN, Tawfik LK, et al. Lip repositioning with or without myotomy: A randomized clinical trial. J Periodontol 2018;89:815–823.
Alammar A, Heshmeh O, Mounajjed R, Goodson M, Hamadah O. A comparison between modified and conventional surgical techniques for surgical lip repositioning in the management of the gummy smile. J Esthet Restor Dent 2018;30:523–531.


