Histopathology of the temporomandibular joint disc: Findings in 30 samples from joints with degenerative disease
ABSTRACT
Aim: The aim of this study is to show the anatomical and histological features of the displaced temporomandibular joint (TMJ) disc in joints with degenerative disease.
Methods: This study was performed on a total of 30 TMJ discs extracted from 22 patients, who underwent surgical discectomy after failure of conservative non-surgical treatment regimens to control pain and/or limited range of motion. All joints had imaging signs of an anteriorized disc position and degenerative joint disease. Samples of the extracted discs were stored in formalin, cut into 3 micron-thick sections imbedded in paraffin and processed with hematoxylin-eosin.
Result: All the samples present irreversible morphologic and histological alterations. The macroscopical evaluation showed that 14 discs were worn and fragmented in several parts, and one disc was perforated. Morphological alterations with deformation and degenerative signs were shown in all discs, which were all severely worn and compromised. Histologically, various alterations were found, such as pre-fibrous sclerosis with myxoid degeneration and collagen deposits (N = 25), an increase in fibrohyaline and fibrous tissues, with loss of elasticity (N = 25), scattered calcifications (N = 15), and synovial inflammation with microvascular proliferation and increased cellularity, presence of lymphocytes, histiocytes and plasma cells (N = 18). After the intervention, all patients reported decreased pain levels and showed improved function at 6 months.
Conclusion: These observations suggest that degenerative joint disease is accompanied by a anteriorized discs featuring abnormal macroscopical and histological changes. From a clinical viewpoint, this may suggest that, when treatment escalation leads to consider TMJ surgery, total discectomy is the most reasonable approach.
INTRODUCTION
For many years, the clinical relevance of temporomandibular joint (TMJ) disc position in patients with signs and symptoms of degenerative disease has been the topic of debate.1,2 In particular, when escalation to surgical treatment is considered, the choice between removal (i.e., discectomy) and repositioning of the articular disc has been challenging.3,4 TMJ degenerative disease is a progressive condition, which predominantly affects women aged over 40 years, has a chronic, fluctuating but generally favourable course and may be associated with psychosocial impairment.5–8
At the tissue level, the condition is first characterized by a gradual degeneration of superficial articular cartilage and bone surfaces, leading to sclerosis or ischemia with aseptic necrosis. Osteophytic beaks and bone shape changes can then be found, with an alternation of areas of bone production and osteolysis. Over time, involvement of the subchondral bone can be observed, with or without pseudocysts.9–11 Clinically, patients complain of crepitus sounds during mandibular movements and possible painful limitation.12,13
As far as the structure of the articular discs in patients with TMJ arthrosis is concerned, there is a loss of the normal histological pattern. Typically, the physiological disc is characterized by a homogeneous fibrocartilaginous tissue, with isolated or small groups of chondrocytes, separated from each other by a matrix rich in elongated and compact collagen fibers. A degenerated disc may have several types of alterations in its fibrous structure, with possible thickening or lacunae in the collagen matrix, calcifications, fibrosclerosis, and possible vacuolation or mixoid degeneration. The disc itself may lose its integrity, shape and anatomical location, and may interfere with jaw movements (e.g., disc displacement with or without reduction).
Further details about temporomandibular disorders management are accessible for you to learn in our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
All the above structural and histological changes, which are typically identifiable in a severe picture of osteoarthrosis, are de facto irreversible and usually accompanied by the presence of inflammatory molecules in the synovial fluid all around the disc structure.14–17
Despite the favourable natural course and good response to conservative treatments,18–20 a minority of patients with TMJ internal derangements are unable to manage pain symptoms and restore acceptable jaw function with conservative or minimally invasive therapies. In these cases, possible escalation to surgery should be considered, letting the debate open about the possibility and need to try recapturing or preserving the disc for a smooth jaw function.21,22
Within these premises, the aim of this study is to show the anatomical and histological features of the displaced temporomandibular joint disc in joints with degenerative disease and to discuss their possible clinical implications for the debate on disc repositioning. Pictorial correlation with magnetic resonance imaging (MRI) is also described with some example cases.
MATERIALS AND METHODS
This study was performed at the Departments of Oral and Maxillofacial Surgery and of Pathological Anatomy of the Hospital of Treviso, Italy, with the coooperation of the Tissue Bank of Treviso. It received the approval of the local Ethical Committee. The sample included a total of 30 articular discs extracted from 22 patients, aged between 24 and 68 years (20 females).
Patients underwent discectomy after failure of conservative treatment regimens to restore jaw function and provide pain relief. At the clinical examination, all patients had pain during mandible movements and 15 of them also had severe functional limitation or jaw lock. Imaging showed that all patients had severe joint disease (i.e., Wilkes stage 3 or 4). Magnetic Resonance Imaging (MRI of the mandibular condyles, T1 and T2 weighted, with mouth closed and at maximum opening, sagittal and coronal cuts)23–25 showed disc displacement and deformation, along with alterations of the bony heads.
As per routine conservative protocols, all patients were first given instructions for behavioral hygiene as well as passive and active physiotherapy. In 13 individuals, a cycle of five weekly arthrocentesis with hyaluronic acid positioning was performed without any benefits (Sinovial Mini® 0,8% 1 ml 8 mg for unilateral infiltrations or Sinovial® 0.8% 2 ml 16 mg for bilateral infiltrations) in addition to sessions of physiotherapy and behavioral hygiene.
Two of the other patients underwent a single arthrocentesis session to try solving a closed lock, without positioning any drug or medication. The other five patients were wearing an oral appliance delivered by a specialist dentist, and no further interventions besides physiotherapy and behavioral hygiene were planned. After up to 6-to-12 months of lack of improvement, the patients were planned for TMJ surgery. Human amniotic membrane (HAM) was positioned between the bone surfaces to replace the extracted disc.26–28 The discs were stored in formalin (4% formaldehyde) and sent to the pathological anatomy department for histological analysis. The samples were cut into 3 micron-thick sections from the formalin-preserved, paraffin-embedded tissues. Then, the samples were processed with hematoxylin-eosin stain and examined under a microscope.
From a clinical viewpoint, patients were monitored for 6 months after surgery, and re-evaluated for pain levels and mouth opening values. As per the article’s aim, a descriptive analysis of the extracted discs was provided.
RESULTS
The samples of the extracted disc were evaluated both macroscopically and histologically.
The main findings of the macroscopical evaluation concern the presence of 15 hypotrophic and severely worn discs, 14 discs fragmented in several parts, and a perforated disc. Morphological alterations, with deformation and degenerative signs, were shown in all discs, often associated with macroscopically observable bone and condyle alterations.
Hematoxylin-eosin staining allowed to highlight important histological changes:
Histological changes characteristic of an initial arthrosic alteration, with myxoid degeneration and collagen deposits, which usually precedes fibrous sclerosis, were shown in 25 samples;
An increase in fibro-hyaline and fibrous tissues, with loss of elasticity, which indicates a more advanced stage of degeneration, was shown in 25 samples;
Synovial inflammation was shown in 18 samples. Inflammation occurred with microvascular proliferation and increased cellularity, presence of lymphocytes, histiocytes and plasma cells;
Scattered calcifications were shown in 15 samples;
No discs were free from alterations and multiple histological changes were present in all discs.
Features of each sample are described in Table 1.
The figures show some examples of histological changes and the related MR image, for pictorial purposes: ischemia damage in a hypotrophic disc (Figure 1), bilateral pseudocystic degeneration in broken or several damaged discs (Figure 2), lymphoplasmacellular subsyno-vial inflammation in a plicated disc (Figure 3), chondroid metaplasia in a perforated disc (Figure 4), myxoid degeneration in a worn and fragmented disc (Figure 5).
TABLE 1 Features of each patient and specimen samples included in the study
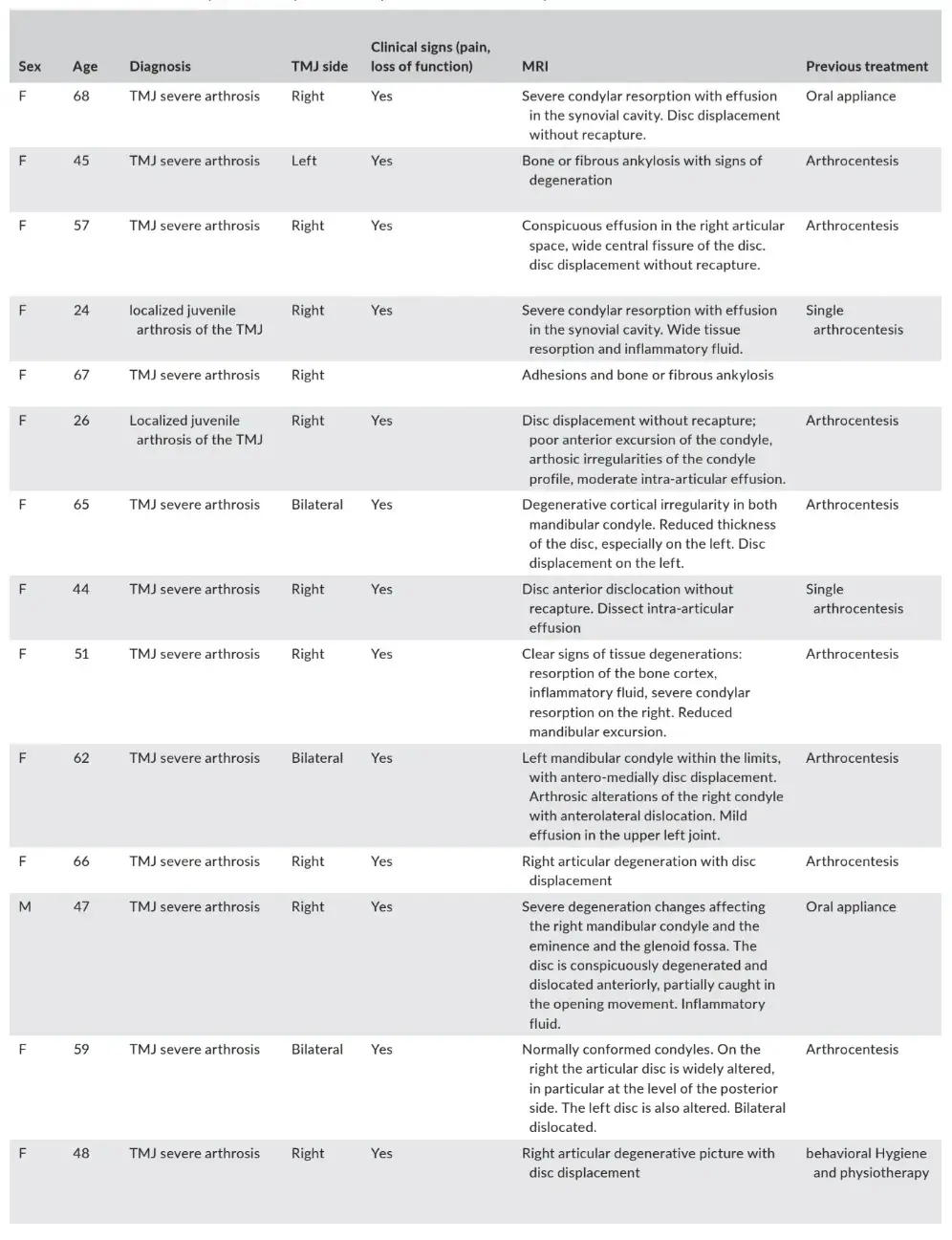
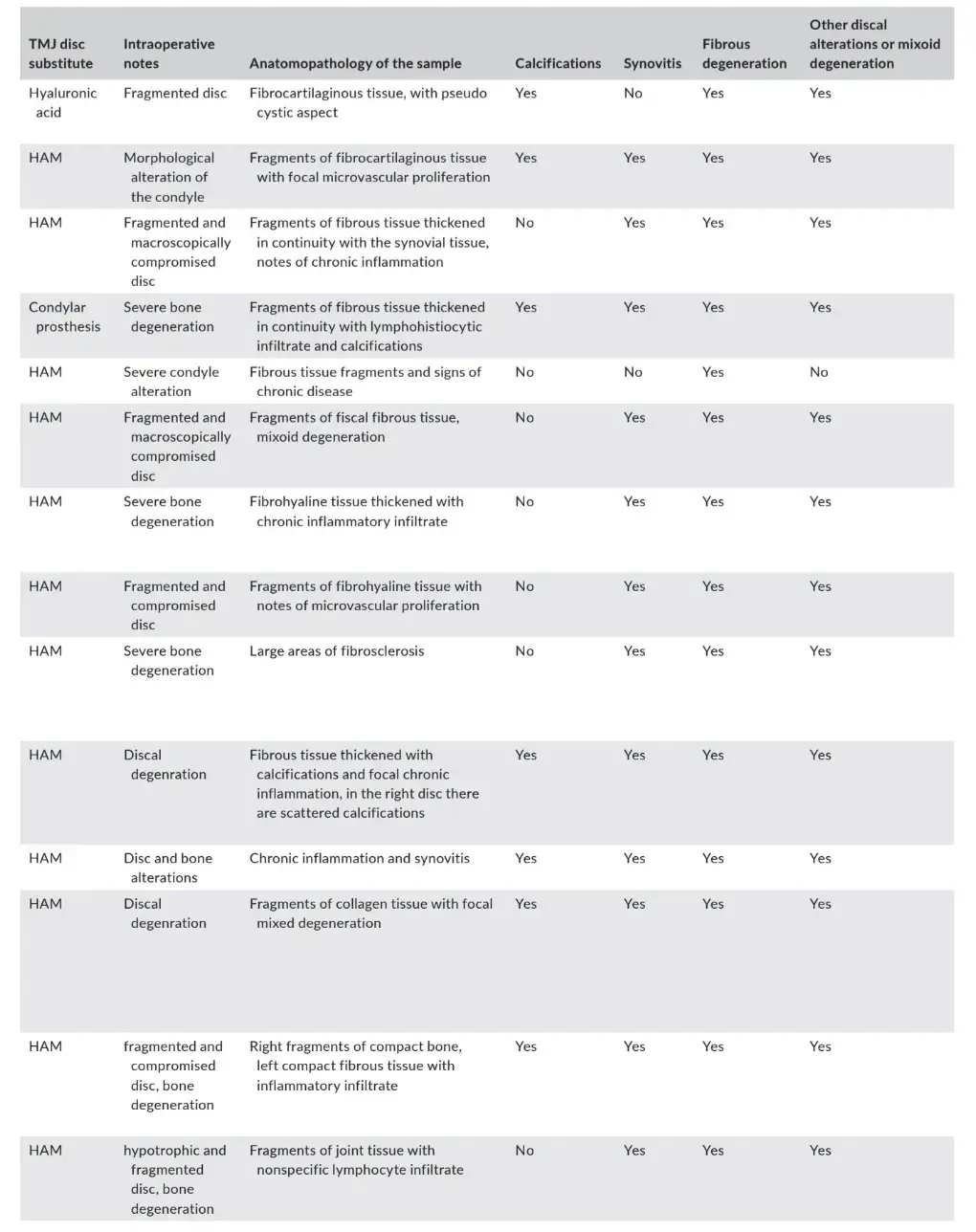
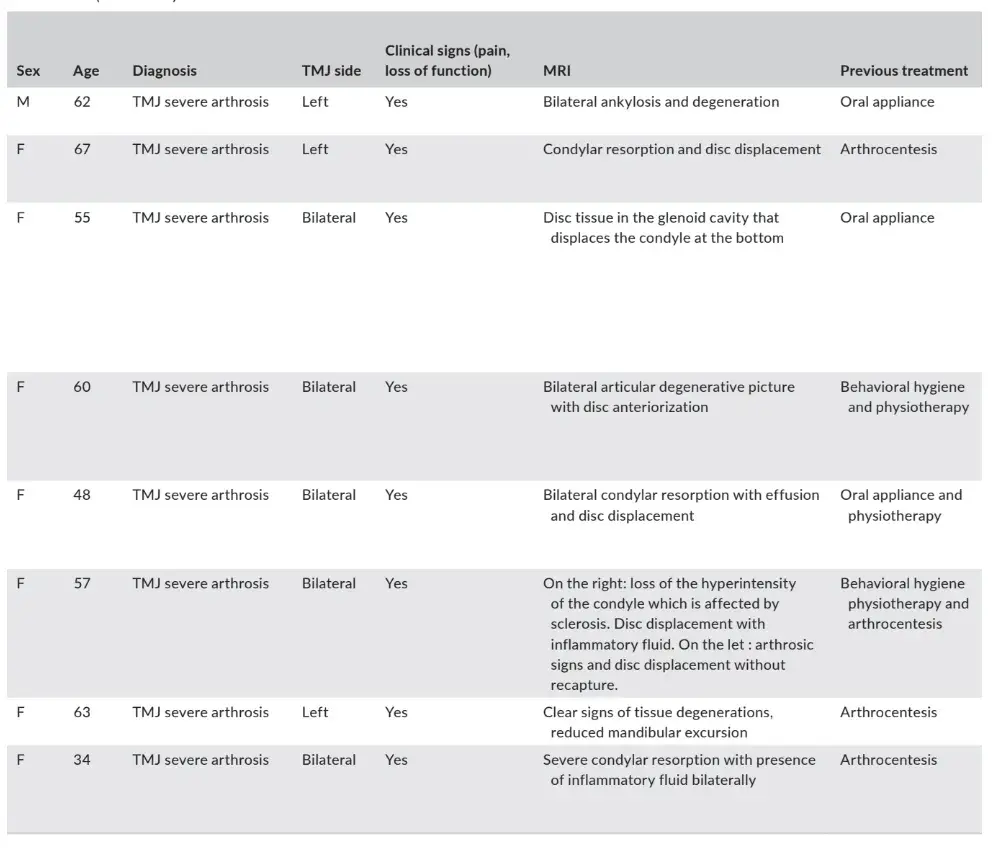
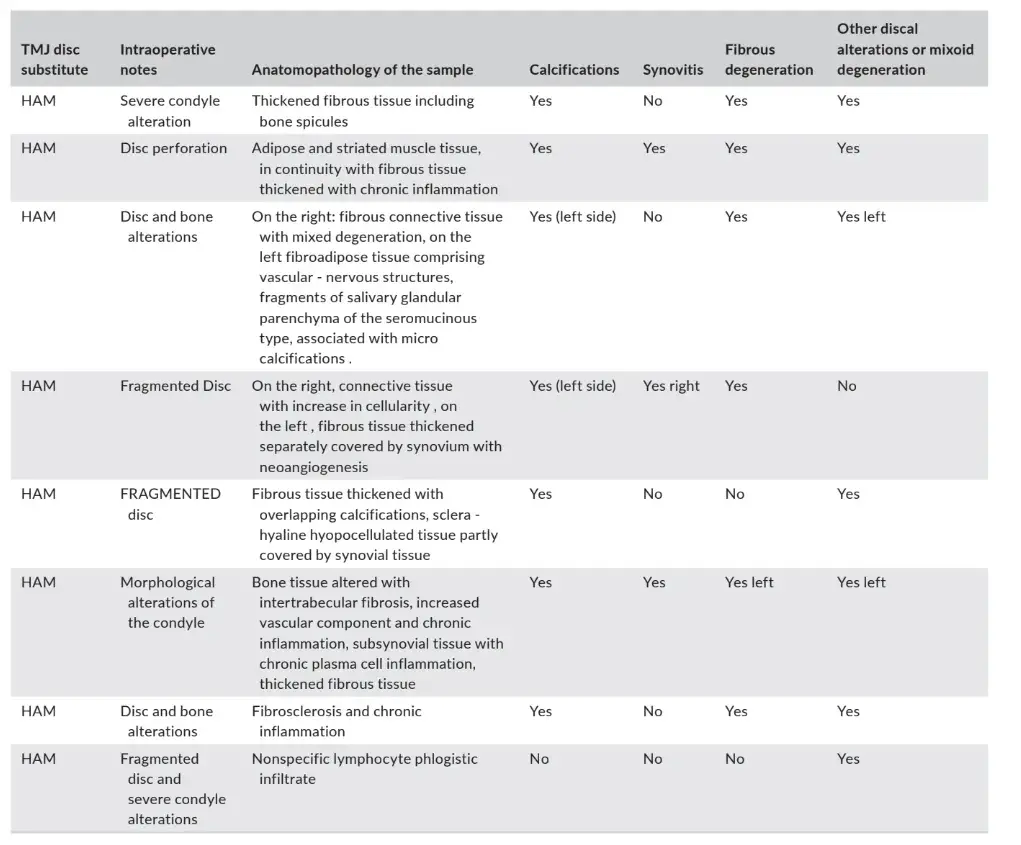
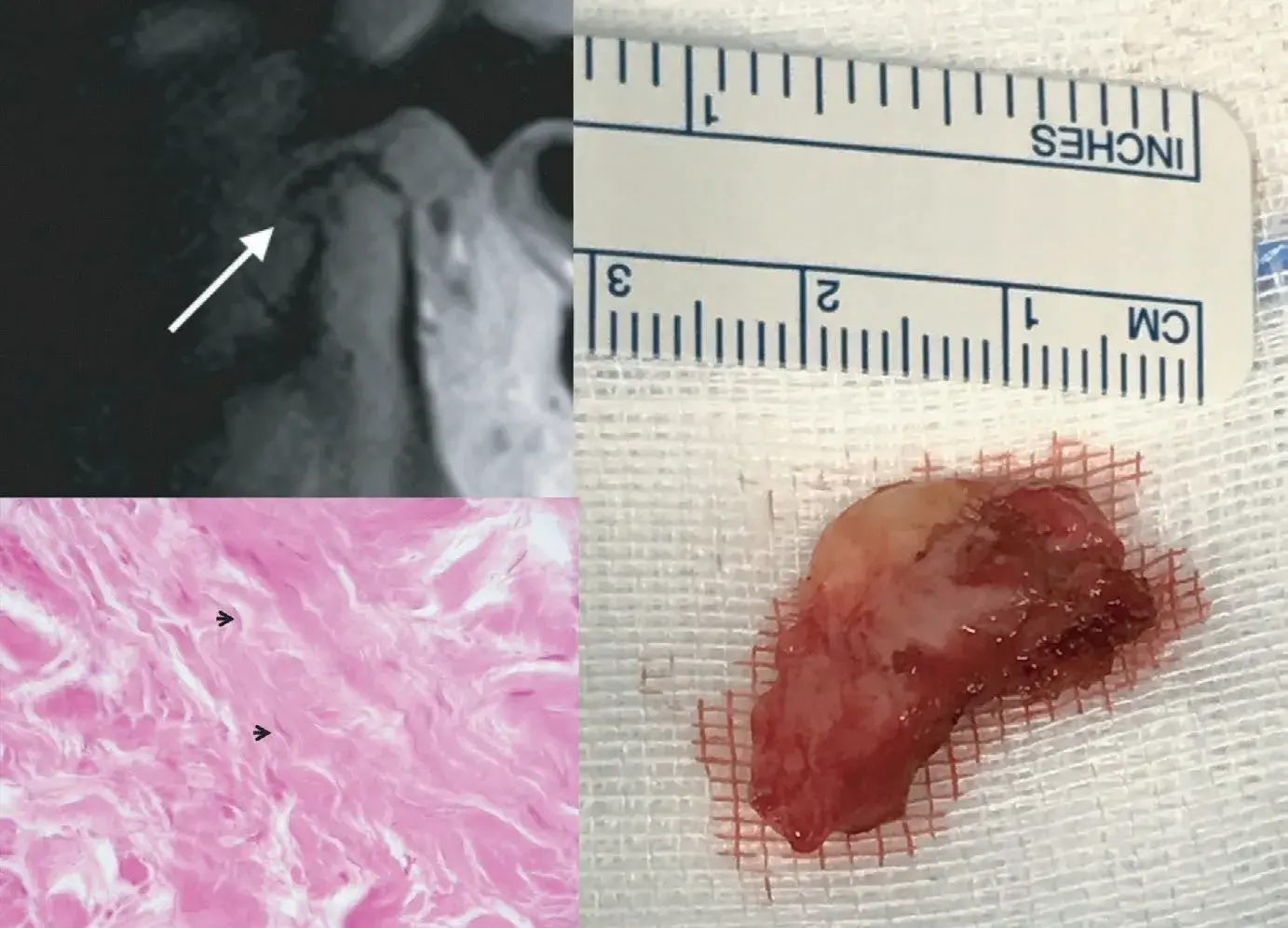 FIGURE 1 Pooled panel. Histological findings show ischemic damage seen as ghost cells; nuclei are barely recognizable (arrow; haematoxylin eosin stain. Original magnification 60x) (A). MRI in the sagittal view shows severe condylar and disc degeneration (B). Surgical specimen of a disc reduced in size and deformed in shape (C)
FIGURE 1 Pooled panel. Histological findings show ischemic damage seen as ghost cells; nuclei are barely recognizable (arrow; haematoxylin eosin stain. Original magnification 60x) (A). MRI in the sagittal view shows severe condylar and disc degeneration (B). Surgical specimen of a disc reduced in size and deformed in shape (C)
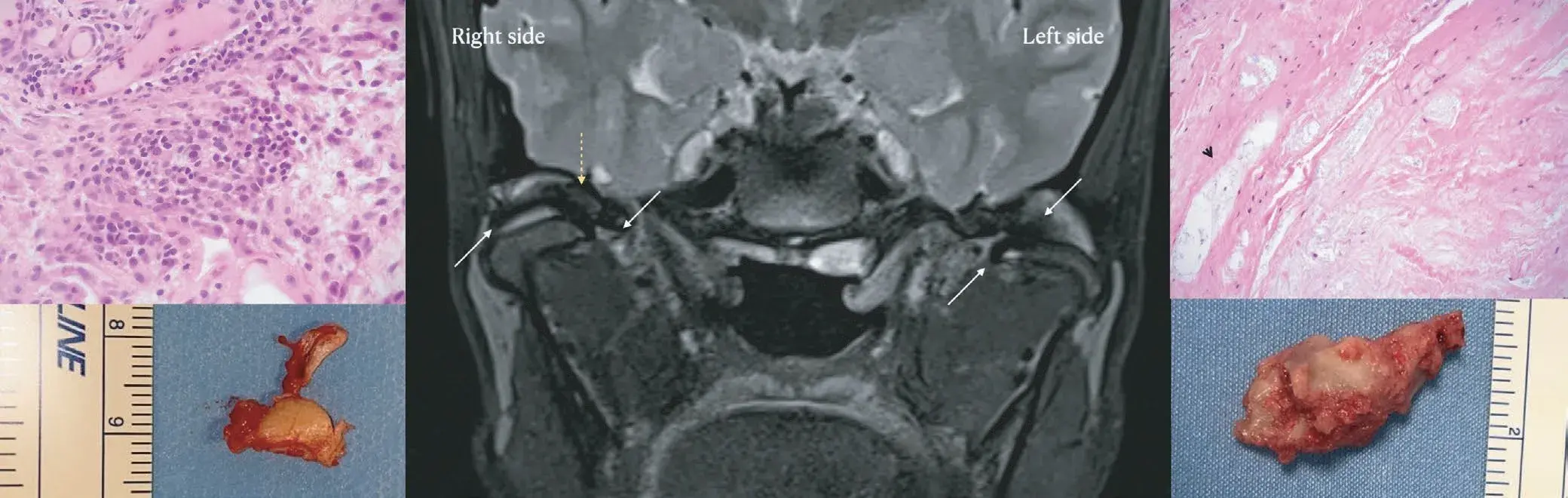 FIGURE 2 Pooled panel of a bilateral sample. Histological findings show in the right side synovial proliferation with inflammation and highly vascularised tissue (haematoxylin-eosin stain, original magnification 40x) (A). On the left side severe myxoid degeneration is shown as deposition of amorphic basophilic substance, with microcystic degeneration (arrow; haematoxylin-eosin stain. Original magnification 60x) (B). MRI in the frontal view shows bilateral effusion (C). Surgical specimen show a broken right disc (D) and severely deformed left disc (E)
FIGURE 2 Pooled panel of a bilateral sample. Histological findings show in the right side synovial proliferation with inflammation and highly vascularised tissue (haematoxylin-eosin stain, original magnification 40x) (A). On the left side severe myxoid degeneration is shown as deposition of amorphic basophilic substance, with microcystic degeneration (arrow; haematoxylin-eosin stain. Original magnification 60x) (B). MRI in the frontal view shows bilateral effusion (C). Surgical specimen show a broken right disc (D) and severely deformed left disc (E)
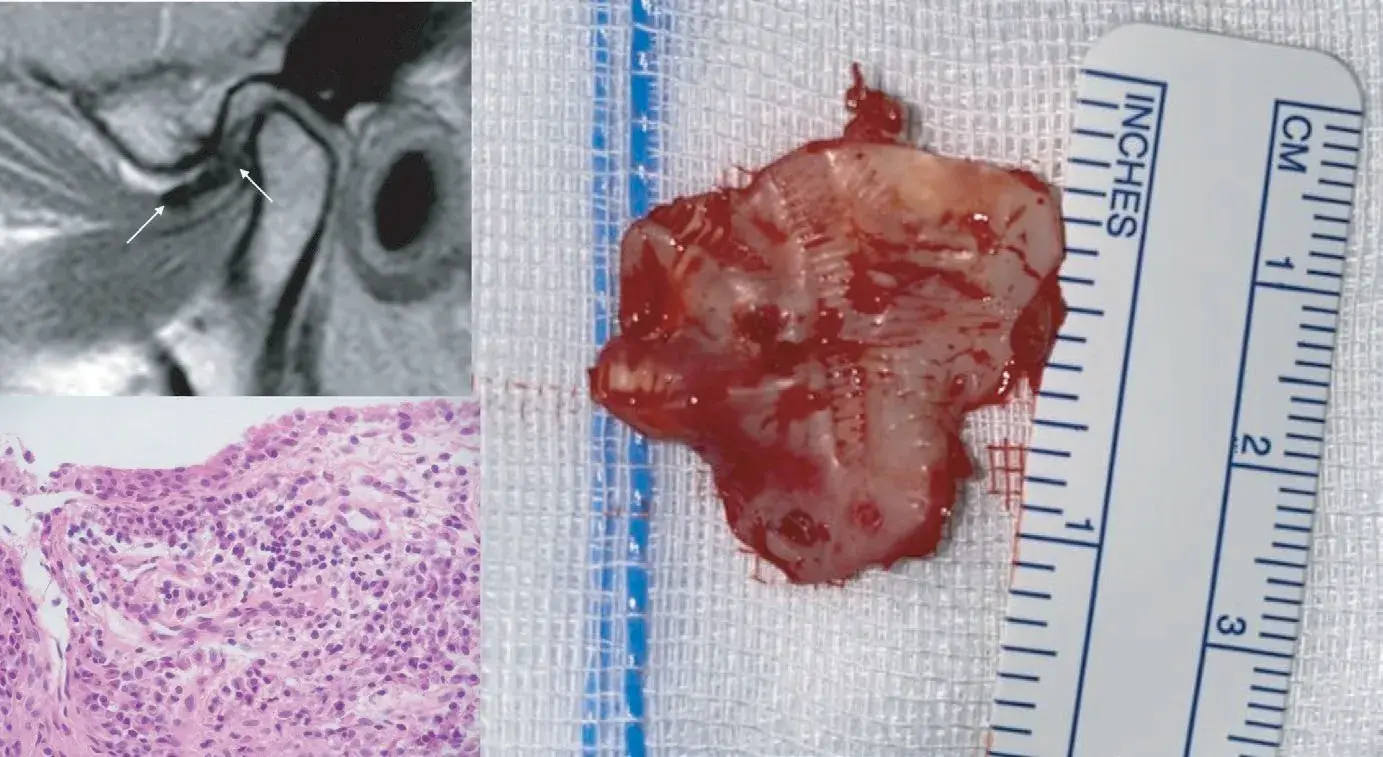 FIGURE 3 Pooled panel. Mild-moderate lymphoplasmacellular subsynovial inflammation is visible histologically (arrow; haematoxylin eosin stain. Original magnification 60x) (A). MRI in the sagittal view shows a displaced disc and a large amount of inflammatory fluid in the antero-superior joint compartment (B). Surgical specimen of a plicated and deformed disc (C)
FIGURE 3 Pooled panel. Mild-moderate lymphoplasmacellular subsynovial inflammation is visible histologically (arrow; haematoxylin eosin stain. Original magnification 60x) (A). MRI in the sagittal view shows a displaced disc and a large amount of inflammatory fluid in the antero-superior joint compartment (B). Surgical specimen of a plicated and deformed disc (C)
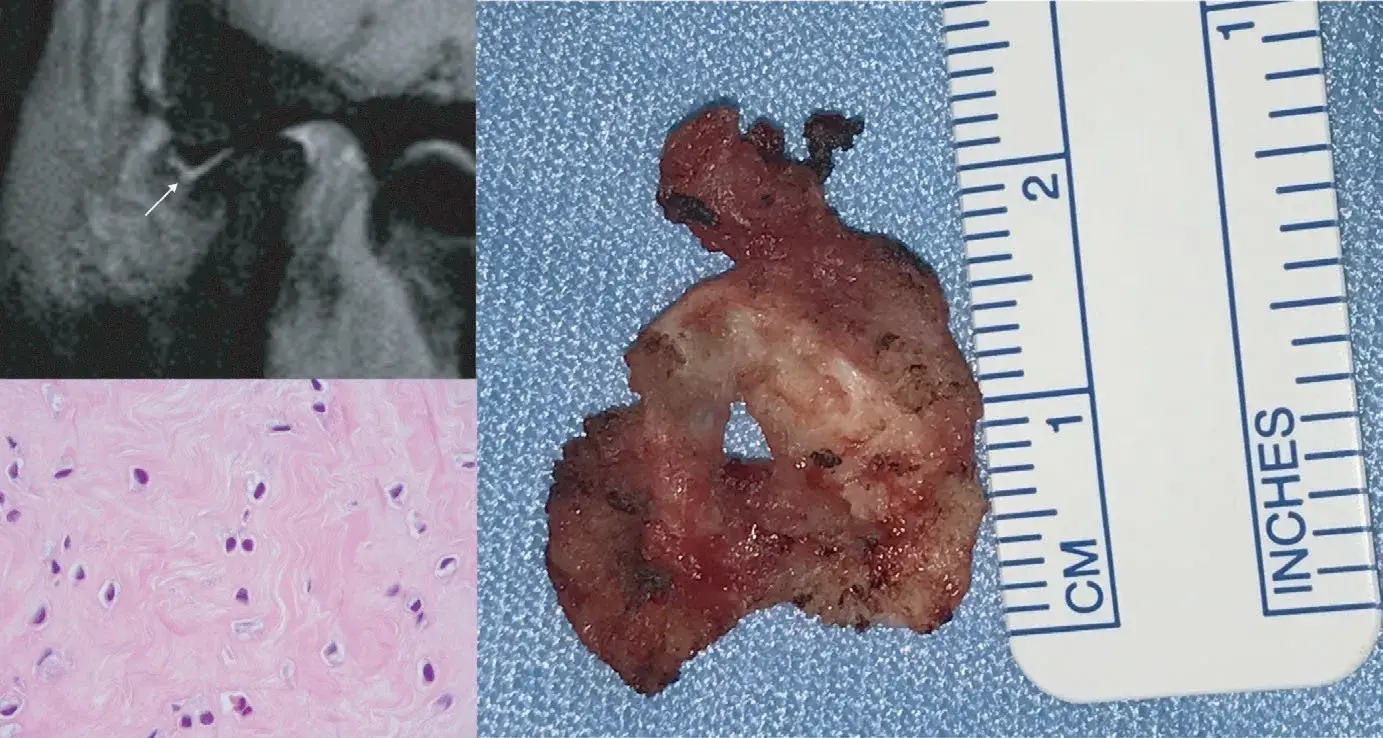 FIGURE 4 Pooled panel showing an example case of a disc with marked chondroid metaplasia. Several chondrocytes are evident (arrow; haematoxylin eosin stain. Original magnification 60x) (A). MRI in the sagittal view shows inflammatory fluid as well as severe disc degeneration, with direct contact between the glenoid fossa and the condylar head (B). Perforation of the disc is visible in the surgical specimen (C
FIGURE 4 Pooled panel showing an example case of a disc with marked chondroid metaplasia. Several chondrocytes are evident (arrow; haematoxylin eosin stain. Original magnification 60x) (A). MRI in the sagittal view shows inflammatory fluid as well as severe disc degeneration, with direct contact between the glenoid fossa and the condylar head (B). Perforation of the disc is visible in the surgical specimen (C
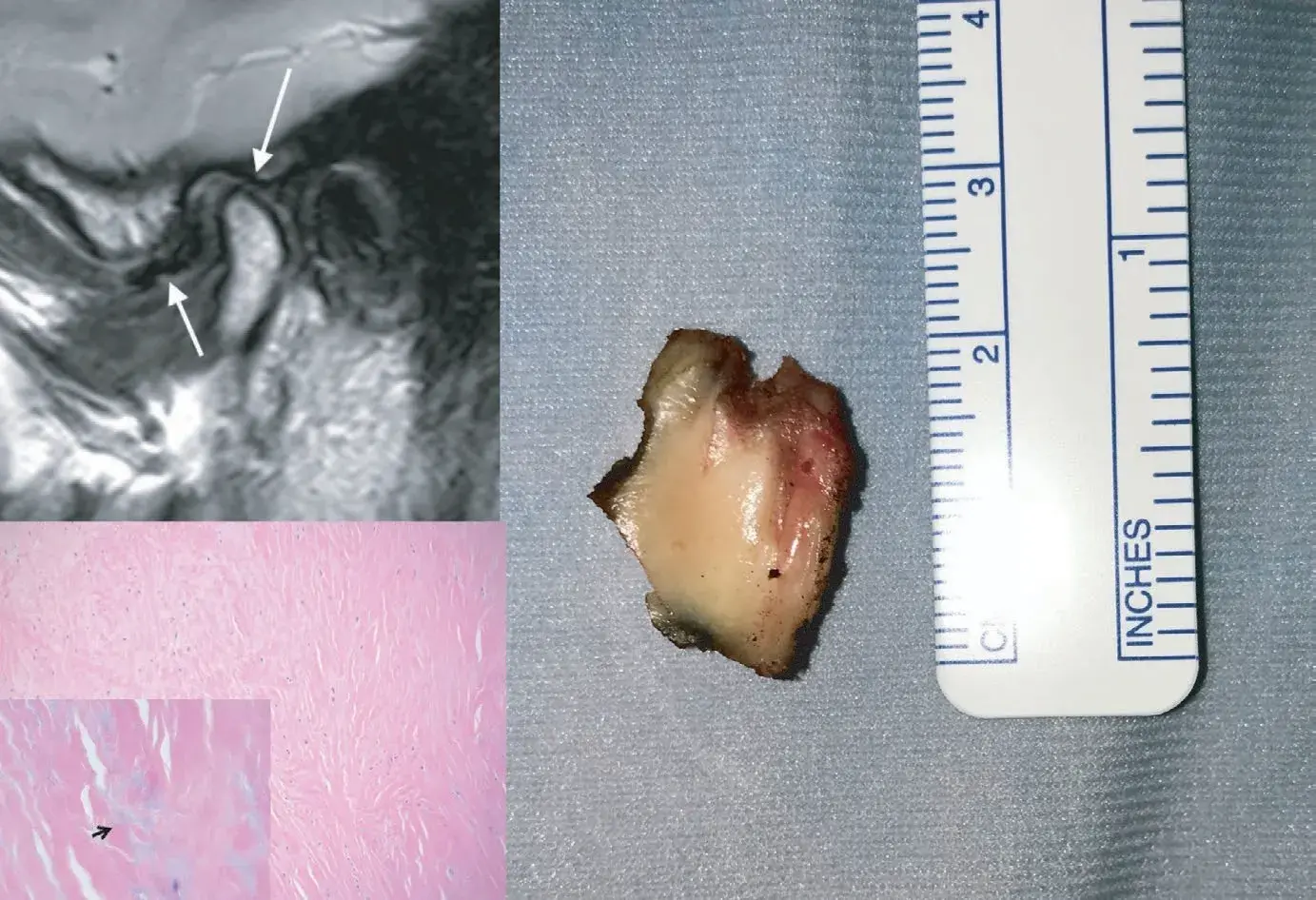 FIGURE 5 Pooled panel. Myxoid degeneration is shown as deposition of amorphic basophilic substance (arrow; haematoxylin eosin stain. Original magnification 20x; insert 60x) (A). MRI shows a displaced disc with initial signs of fragmentation (B). Surgical specimen of a fragmented disc (C)
FIGURE 5 Pooled panel. Myxoid degeneration is shown as deposition of amorphic basophilic substance (arrow; haematoxylin eosin stain. Original magnification 20x; insert 60x) (A). MRI shows a displaced disc with initial signs of fragmentation (B). Surgical specimen of a fragmented disc (C)
DISCUSSION
In the field of TMJ disorders management, escalation to surgery may be needed in selected cases of failure of conservative treatment. In those cases, discectomy offers the possibility of resuming mandibular movement and reducing pain. It can be accompanied by the reasons placement of the disc with different materials. Complete discectomy was one of the first intra-articular TMJ procedures that has been described in the history of medicine and dates back to the early years of the past century. The effectiveness of the procedure has been supported since decades ago, but it seems that there is still some debate about the possibility and need to preserve the disc in some cases.
Similar concerns exist for the management of disc displacement in the dental office, where the so-called “Third Pathway” for TMD treatment (i.e., mandible repositioning strategies) seems to be still practiced by some communities of clinicians. Thus, this study was performed with the aim to provide an insight into the histological changes of displaced discs in joints with signs of degenerative disease, for possible addition to the discussion on the topic. Some pictorial examples of correlation between the extracted disc and the corresponding imaging findings were also provided for descriptive purposes.
The literature on the predictive factors for positive outcomes of TMJ disc surgery is not conclusive, since case series seem to support the effectiveness of both disc removal and disc repositioning strategies to provide adequate pain relief and improve jaw function in selected patients. An early study with a long-term follow-up of nearly 30 years after discectomy, all 15 patients declared themselves pain-free and did not perceive any problems with mandibular dysfunction.29 In another study with a 30-year follow-up, 96% of patients had no pain after surgery and had a maximum interincisal opening greater than or equal to 30 mm.30
Successful outcomes at very long follow up were reported also by another paper.31 Nonetheless, clinical studies involved few patients and were performed by the same few clinicians. In parallel, some authors proposed that displaced TMJ discs might be repositioned or preserved with good outcomes, thus questioning the need to extract the disc during TMJ surgery procedures.
Concerning disc repositioning, findings have been reported in some case series and few comparative trials. One of the largest case series described the results in 105 patients with early stage Wiles disease (i.e., stage 1 or 2) followed up for at least 1 year, describing a significant improvement in terms of pain and joint noise reduction.32 After disc repositioning procedures, there was an increase in mouth opening, even if lateral movements were not well preserved, as an inevitable consequence of disc fixation. Patients with a history of long-lasting disc displacement (i.e., more than 4 years) had a poorer outcome (68% of success) than those with more recent disc displacement (90% of success). Of notice, clinical evaluation of treatment outcomes has been seldom accompanied by postoperative MRI to show the long-lasting stability of disc repositioning and to associate it with pain relief. To this purpose, a smaller case series of 23 joints showed the persistence or reoccurrence of disc displacement after their repositioning in 48% of joints.33 An interesting study compared three different surgical techniques: discoplasty, discectomy without disc replacement, discectomy with Teflon-Proplast disc replacement.34 After 5 years, 94% of patients who underwent discectomy reported decrease of symptoms, whilst the group treated with discoplasty showed a high frequency of recurrences, requiring a second surgery. When the need for re-intervention emerged in this group, patients underwent discectomy with or without replacement of the disc.
The literature on the management of disc displacement with the use of oral appliances to recapture the disc is equally discordant. In general, studies on repositioning strategies are limited to early papers on the use of anterior repositioning appliances (ARA) to try recapturing the disc and improve symptoms in patients with disc displacement with reduction.35–38 Some investigations reported that joint sounds can be reduced more with ARA than flat appliances, which is an implicitly obvious finding based on the rationale of using ARA to place the condyle under the displaced disc.
However, no literature is available that confirms the long-term superiority in pain management of any definitive disc repositioning strategies with comparison to conservative approaches in such cases.
In addition, the progressive increase in knowledge on the natural course of TMJ clicks has shown that most of them do not progress to become a more serious TMJ disorder.39,40 Thus, the available evidence suggests that TMJ repositioning has not been proven necessary in treating either simple muscle or joint TMDs, nor for the long-term treatment of displaced disc conditions (i.e., disc recapture), even after decades of practice.2
Taken together, these data suggest that achieving a position of the disc over the condylar head is not necessarily a fundamental target for treatments aiming at pain relief and functional improvement. Along with the diminished indications for TMJ surgery as a whole, they contributed to a progressive decline of disc repositioning surgeries as well as disc recapturing appliances.
Within these premises, this investigation added some info by evaluating the histological and anatomical features of displaced discs in joints with severe degeneration. Our specimen confirmed that disc displacement is not, as per its definition, just a displacement. Displaced discs feature some macro-(i.e., anatomical) and microscopic (i.e., histological) changes that were already hypothesised by other authors.41 In particular, there was no disc with a preserved integrity. Generalized worn, fragmentation, jagged edge, calcification, inflammation were quite common findings in this study sample, which may require a future investigation for the possible identification of any specific correlation with MRI and clinical findings, which were out of the purposes of this investigation. The presence of such signs of disc degeneration put into serious doubt the rationale for attempting a repositioning when overall joint integrity is compromised. Thus, from an anatomo-histological viewpoint it seems rationale to suggest that, when escalation from conservative treatments leads to consider surgery, discectomy should be the reference intervention concerning the approach to TMJ disc. The surgical choice of preserving and repositioning the disc is interesting, but it may be inconsistent with the concept of the physiology of mandibular movements, with the evidence of the irreversibility of disc degeneration itself with disease progression, and with current knowledge that conservative treatments are enough for most patients with early stage disease. Based on that, it is recommended that the clinical usefulness of disc preservation that can be achieved with some elected surgical strategies and technical showcases performed in the early stages of displacement is supported with respect to conservative treatments. On the other hand, from a biological and clinical viewpoint, the procedures aiming to reposition, by surgery or by using appliances, discs that have undergone deformation and degeneration, and that have irreversibly lost their anatomical identity and intrinsic structure, cannot be supported. To this purpose, orthopedic approaches to knee meniscus should be possibly taken as an example of concrete guidelines.
There are additional resources available to enhance your understanding of the topic of TMJ disorders treatment in our course "Treatment of severe forms of TMJ diseases".
CONCLUSIONS
This histological and anatomical study of joints with severe degeneration showed that patients who are candidates for TMJ surgery present a worn or even perforated disc, with jagged edges, sometimes frowned or crushed towards the direction of displacement. These observations suggest that, when TMJ surgery is required in severely degenerated joints, total discectomy appears as the most reasonable approach based on the histopathological findings of TMJ disc alteration.
References
Naeije M, Te Veldhuis AH, Te Veldhuis EC, Visscher CM, Lobbezoo F. Disc displacement within the human temporomandibular joint: a systematic review of a “noisy annoyance”. J Oral Rehabil. 2013;40:139–158.
Greene CS, Manfredini D. Treating temporomandibular disorders in the 21st century: can we finally eliminate the “Third Pathway”? J Oral Facial Pain Headache. 2020;34:206–216.
Dolwick MF. Intra-articular disc displacement: part I: its questionable role in temporomandibular joint pathology. J Oral Maxillofac Surg. 1995;53:1069–1072.
Hall HD. Intra-articular disc displacement Part II: its significant role in temporomandibular joint pathology. J Oral Maxillofac Surg. 1995;53:1073–1079.
Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiological findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453–462.
De Leeuw R, Boering G, Van der Kuijl B, Stegenga B. Hard and soft tissue imaging of the temporomandibular joint 30 years after the diagnosis of osteoarthritis and internal deranegement. J Oral Maxillofac Surg. 1996;54:1270–1280.
Matos MF, Catunda IS, Matos JL, Vasconcelos BC, Learreta JA. Autoimmune temporomandibular arthropathy: diagnostic considerations. Gen Dent. 2018;66(4):56–61.
Canales GT, Guarda-Nardini L, Rizzatti-Barbosa CM, Conti PCR, Manfredini D. Distribution of depression, somatization and pain-related impairment in patients with chronic temporomandibular disorders. Appl Oral Sci. 2019;7:27.
Emshoff R, Brandlmaier I, Schmid C, Bertram S, Radish A. Bone marrow edema of the mandibular condyle related to internal derangement, osteoarthritis and joint effusion. J Oral Maxillofac Sure. 2003;61:35–40.
Larheim TA, How C, Ottersen MK, Mork-Knutsen BB, Arvidsson LZ. The role of imaging in the diagnosis of temporomandibular joint pathology. Oral Maxillofac Sure Clin North Am. 2018;30:239–249.
Stegenga B. Osteoarthrits of the temporomandibular joint organ and its relationship with disc displacement. J Orofac Pain. 2001;15:193–205.
De Bont LG, Dikkgraaf LC, Stegenga B. Epidemiology and natural progression of articular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:72–76.
Wiese M, Svensson P, Bakke M, et al. Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain. 2008;22:239–251.
Ghassemi Nejad S, Kobezda T, Tar I, Szekanecz Z. Development of temporomandibular joint arthritis: the use of animal models. Joint Bone Spine. 2017;84(2):145–151.
Blaunstein DI, Scapino RP. Remodeling of the temporomandibular joint disk and posterior attachment in disk displacement specimens in relation to glycosaminoglycan content. Last Reconstr Sure. 1986;78:756–764.
Suzuki T, Segami N, Nishimura M, Sato J, Nojima T. Bradykinin expression in synovial tissues and synovial fluids obtained from patients with internal derangement of the temporomandibular joint. Cranio. 2003;21(4):265–270.
Kaneyama K, Segami N, Nishimura M, Sato J, Suzuki T, Fujimura K. Osteoclastogenesis inhibitory factor/osteoprotegerin in synovial fluid from patients with temporomandibular disorders. J Oral Maxillofac Surg. 2003;32(4):404–407.
Manfredini D, Favero L, Cocilovo F, Monici M, Guarda-Nardini L. A comparison trial between three treatment modalities for the management of myofascial pain of jaw muscles: a preliminary study. Cranio. 2018;36(5):327–331.
Manfredini D, Rancitelli D, Ferronato G, Guarda-Nardini L. Arthrocentesis with or without additional drugs in temporomandibular joint inflammatory-degenerative disease: comparison of six treatment protocols. J Oral Rehabil. 2012;39(4):245–251.
Al-Moraissi EA, Wolford LM, Ellis E, Neff A. The hierarchy of different treatments for arthrogenous temporomandibular disorders: a network meta-analysis of randomized clinical trials. Craniomaxillofac Surg. 2020;48(1):9–23.
Goncalves JR, Cassano DS, Rezende L, Wolford LM. Disc repositioning. Does it really work? Oral Maxillofac Sure Clin North Am. 2015;27:85–107.
Renapurkar SK. Discectomy versus disc preservation for internal derangement of the temporomandibular joint. Oral Maxillofac Sure Clin North Am. 2018;30:329–333.
Al-Saleh MA, Alsufyani NA, Saltaji H, Jaremko JL, Major PW. MRI and CBCT image registration of temporomandibular joint: a systematic review. J of Otolaryngol Head Neck Surg. 2016;45(1):30.
Kaimal S, Ahmad M, Kang W, Nixdorf D, Schiffman EL. Diagnostic accuracy of panoramic radiography and MRI for detecting signs of TMJ degenerative joint disease. Gen Dent. 2018;66(4):34–40.
Sano T, Yamamoto M, Okano T, Gokan T, Westesson PL. Common abnormalities in temporomandibular joint imaging. Curr Probl Diagn Radiol. 2004;33(1):16–24.
Guarda-Nardini L, Trojan D, Montagner G, Cogliati E, Bendini M, Manfredini D. Amniotic membrane positioning in the surgical treatment of temporomandibular joint degenerative disorder. Case Rep Surg. 2019; 2019:6037191.
Guarda-Nardini L, Trojan D, Paolin A, Manfredini D. Management of temporomandibular joint degenerative disorders with human amniotic membrane: Hypothesis of action. Med Hypotheses. 2017;104:68–71.
Akhter M, Ahmed N, Arefin MR, Sobhan MU, Molla MR, Kamal M. Outcome of amniotic membrane as an interpositional arthroplasty of TMJ ankylosis. Oral Maxillofac Surg. 2016;20(1):63–71.
Eriksson L, Westesson P-L. Long-term evaluation of meniscectomy of the temporomandibular joint. Oral Maxillofac Surg. 1985;43(4):263–269.
Silver CM. Long-term results of meniscectomy of the temporomandibular joint. Cranio. 1984;3(1):46–57.
Tolvanen M, Oikarinen VJ, Wolf J. A 30-year follow-up study of temporomandibular joint meniscectomies: a report on five patients. J Oral Maxillofac Surg. 1988;26(4):311–316.
Mehra P, Wolford LM. The Mitek mini anchor for TMJ disc repositioning: surgical technique and results. Int J Oral Maxillofac Surg. 2001;30(6):497–503.
Westesson PL, Cohen JM, Tallents RH. Magnetic resonance imaging of temporomandibular joint after surgical treatment of internal derangement. Oral Surg Oral Med Oral Pathol. 1991;71(4):407–411.
Trumpy IG, Lyberg T. Lyberg: surgical treatment of internal derangement of the temporomandibular joint: long-term evaluation of three techniques. J Oral Maxillofac Surg. 1995;53(7):740–746.
Lundh H, Westesson PL, Jisander S, Eriksson L. Disk-repositioning onlays in the treatment of temporomandibular joint disk displacement: comparison with a flat occlusal splint and with no treatment. Oral Surg Oral Med Oral Pathol. 1988;66(2):155–162.
Westesson PL, Lundh H. Temporomandibular joint disk displacement: arthrographic and tomographic follow-up after 6 months' treatment with disk-repositioning onlays. Oral Surg Oral Med Oral Pathol. 1988;66(3):271–278.
Okeson JP. Long-term treatment of disk-interference disorders of the temporomandibular joint with anterior repositioning occlusal splints. J Prosthet Dent. 1988;60(5):611–616.
Anderson GC, Schulte JK, Goodkind RJ. Comparative study of two treatment methods for internal derangement of the temporomandibular joint. J Prosthet Dent. 1985;53(3):392–397.
Greene CS. A critique of nonconventional treatment concepts and procedures for TMJ disorders. Compend Contin Educ Dent. 1984;5(10):848–51, 854.
Zamburlini I, Austin D. Long-term results of appliance therapies in anterior disk displacement with reduction: a review of the literature. Cranio. 1991;9(4):361–368.
Stankovic S, Vlajkovic S, Boskovic M, Radenkovic G, Antic V, Jevremovic D. Morphological and biomechanical features of the temporomandibular joint disc: an overview of recent findings. Arch Oral Biol. 2013;58:1475–1482.


